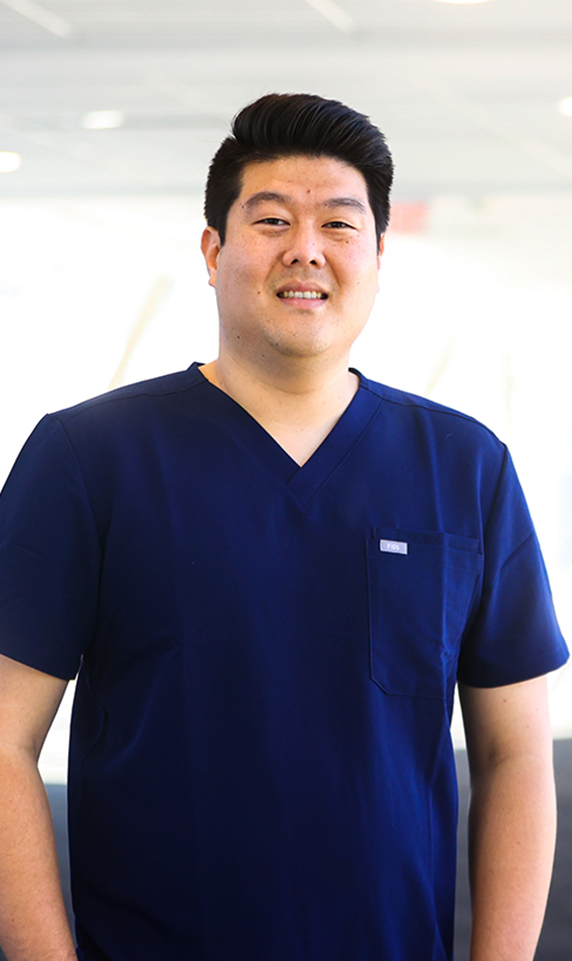

PHARMACISTS UP CLOSE
Alex Kim, PharmD, PGY 1
“I realized that I’m a very extroverted and social person. I wanted to do something that included more of that personal connection with people.”
-Dr. Alex Kim
When Dr. Alex Kim, Acute Care Pharmacy Resident at the University of Kentucky’s Albert B. Chandler Hospital walks into a patient’s room, they should know that he’s going to spend some time with them.
It’s a part of his philosophy on how to help patients get the best outcome possible. By taking the time to get to know a patient, he learns how to best tailor their treatment to ensure they can follow through.
“I want to sit down with you and talk. I want to know what the factors are that might be limiting you from taking your medication. I want to know all of this so I can build a regimen around you.”
I want to sit down with you and talk. I want to know what the factors are that might be limiting you from taking your medication.”
As part of his training, Dr. Kim does regular rotations with different specialty care teams. He has worked with patients in the ED and ICU as well as inpatient and outpatient settings. The common thread he has seen is how important a hospital or health-system pharmacist is to maintaining consistent care throughout a patients’ health journey.
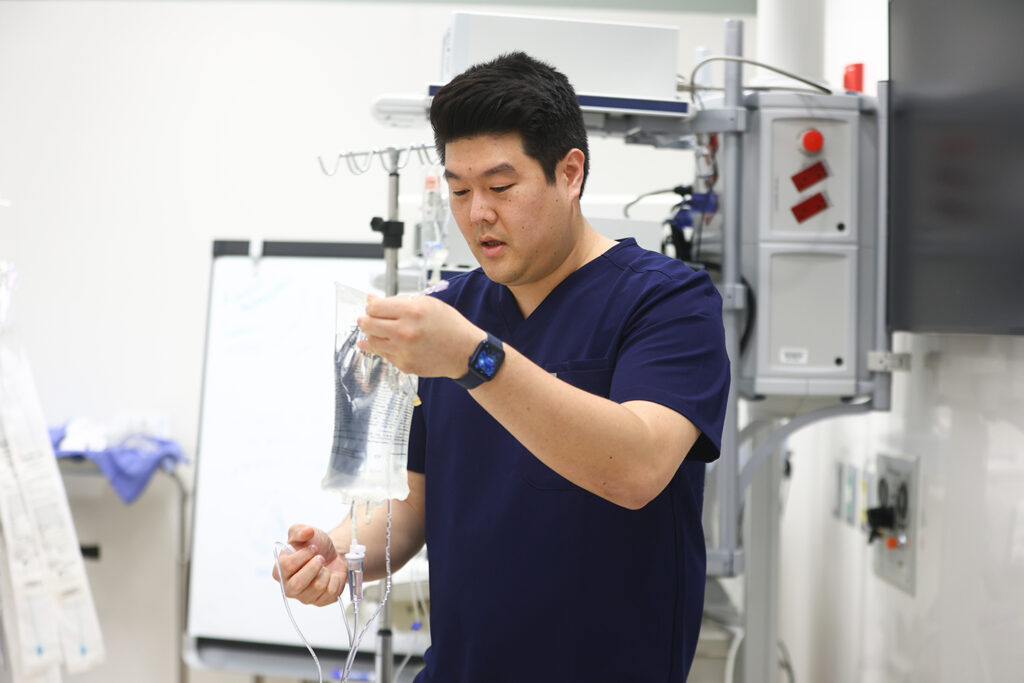

“I’m there when you get admitted working to develop the medication plan, I’m there when you’re discharged making sure you have the medications you need and understand how to use them, and I’m there after you get home checking in with you to make sure that everything is working correctly and that you’re comfortable with following through with your treatment.”

And while Dr. Kim is his patients’ medication expert and advocate throughout their care, he says the time spent learning about patients really pays off when patients are getting ready to go home.
“Let’s say you had a history of blood clots, and you’re using an older blood thinner. Many of those medications require a weekly blood draw. And it adds an additional layer of complexity to your care. So, I start looking for newer alternatives for you, but we realize your insurance won’t cover the newer drugs or the newer copay is going to put you in a financial crunch. I’ll go to our prior authorization team to help find a medication that is more aligned to your situation and work with manufacturers to find coupons to help keep your costs lower. But, I wouldn’t have known to do this if I didn’t take the time to talk to you and learn about you personally, not just your condition.”
I wouldn’t have known to do this if I didn’t take the time to talk to you and learn about you personally, not just your condition.”
Dr. Kim said that as a resident he’s learned how valuable it is to have a hospital or health-system pharmacist as that connector between care teams, social workers and patients. His experiences being at the center of the patients’ journey is, in his opinion, the best part of being a hospital or health-system pharmacist.
“The most rewarding part of my job is that at the end of the day, I know that I helped you get better. When you come to the hospital, I understand how you must feel. You need someone who is there for you, who is working with everyone who is caring for you, and is cheering for you as a person, not just a patient.”
For Dr. Kim, that’s what it means to make a personal connection, and what it means to be your pharmacist.